 Figure 1 (Click for full image)
Figure 1 (Click for full image)
The Middle-Class Plague:
Epidemic Polio and the Canadian
State, 1936-1937*
By CHRISTOPHER J. RUTTY, Ph.D.
HEALTH
HERITAGE RESEARCH SERVICES
96 Durie Street, Toronto, Ontario, Canada, M6S 3E9
http://www.healthheritageresearch.com
hhrs@healthheritageresearch.com
© Christopher J. Rutty, 1999
Originally published in the Canadian
Bulletin of Medical History 13 (1996): 277-314
View the original article as a pdf file
Click here for online access to all issues of the Canadian Bulletin of Medical History
PAGE INDEX:
ABSTRACT | POLIO
IN THE CANADIAN CONTEXT | Second Wave
Epidemics & the Provincial Public Health Response | PREVENTION
& TREATMENT METHODS IN CANADA: "Paralysis Nose Spray: Just Squirt &
Smile" | "Miraculous Metal Monsters"
| Standardized Treatment, Hospitalization & Aftercare
| CONCLUSIONS | ENDNOTES
Figure 1 | Figure 2
| Figure 3 |
Table 1 | Table 2 | Table
3 |
During the pre-Salk era, paralytic poliomyelitis was one of the most feared diseases of twentieth-century North America. This perception, held most strongly by the middle class -- polio’s principal target -- shaped a unique Canadian response to it based on comprehensive, standardized and unconditional programs of "state medicine" at the provincial level. Of Canada’s four major waves of provincial polio epidemics, the second struck Ontario to an unprecedented degree in 1937, generating a similarly unprecedented response from the Ontario government in its control, treatment, hospitalization and after-care measures. As this article discusses, the severity of this epidemic led the provincial, and other Canadian public health authorities, to face a central question: How far should governments be compelled to go to ensure the advantages of modern treatment for their people? This article helps place the social impact of, and political and scientific response to, epidemic polio within the context of Canada’s evolving public health and state medicine infrastructure at the time.
Until the Salk and Sabin vaccines were introduced in 1955 and 1962, respectively, paralytic poliomyelitis was one of the most feared diseases of twentieth-century North America. Indeed, during the two or three decades before 1955, parents told their children to "to regard [polio] as a fierce monster that lurked in the damp hollows of their experience," and personified the disease as "a grim terror... more menacing, more sinister than death itself."(1) This frightening imagery, generated and magnified each summer -- "polio season" -- by the popular press, shaped a unique Canadian response to this disease. In fact, polio’s dramatic threat and associated paralysis striking otherwise healthy middle class children was more significant to its public management than its actual prevalence relative to other, more deadly, diseases of the period. Indeed, as Richard Carter stressed in his study of American voluntary health organizations, one could reassure the public that polio was "a comparatively rare disease hardly worth all the razzmatazz... but you could not convince them, because they knew from experience that nothing was more frightening or tragic than a polio epidemic."(2)
This climate of fear was reinforced by the sharply rising incidence of epidemic polio during the first half of the century, especially among middle class families living in the "better areas," and by the fact that little to nothing could be done to prevent "the crippler" until polio vaccines were widely used. There is still no cure for polio’s paralytic effects, nor for the post-polio syndrome that is now forcing many polio survivors to fight the disease, physically and psychologically, all over again.(3) In a context of celebrated success in combating many other infectious disease by the early decades of the twentieth, the Canadian medical profession frequently acknowledged a profound helplessness with respect to polio. For example, in 1936, an article in the Manitoba Medical Association Review declared that "There is no disease over which the public is more apprehensive and in which both the laity and the medical profession feel so helpless than Epidemic Poliomyelitis."(4) Thus, despite medical science -- and, ironically, because of improving public health and personal hygiene standards that delayed what had earlier been an endemic, invisible, harmless and almost universal gastrointestinal infection -- during the first half of this century epidemics of paralytic polio escalated throughout the industrialized world. For geographic, demographic and epidemiological reasons, Canada was particularly vulnerable.
The many serious polio epidemics that have occurred between the late 1920s and early 1950s have received minimal historical attention. Most studies of this disease have focused on the American scene surrounding the Salk vaccine story;(5) on the major epidemics of earlier decades, especially the great 1916 Northeastern U.S. epidemic;(6) or on the personal experience of polio victims, especially the most famous one, Franklin D. Roosevelt.(7) Until quite recently, no comprehensive national study of polio had been attempted, nor had many Canadian studies been written.(8) This article forms part of a national study that places the social impact of, and public response to, epidemic polio during the 1930s within the context of Canada’s evolving public health and state medicine infrastructure before the development public hospital and medical insurance.
The nature of the state’s response to polio was mitigated, in general, by recognized local and national traditions of public health activity, the relationship of governments and public health authorities with the medical profession, and the level of activity among voluntary organizations and individuals.(9) In the United States, the emphasis was on philanthropic, individual, and especially voluntary support for polio victims, and not on governments. This direction was reinforced by Roosevelt’s experience with polio in 1921 and, after his 1932 election as President, his establishment of the National Foundation for Infantile Paralysis, or "March of Dimes in 1938."(10) In the same period, however, and in many ways in reaction to the American approach, an opposite strategy to the polio problem developed in Canada.
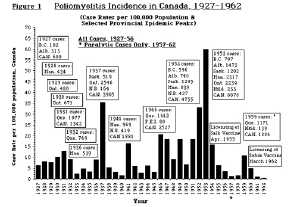 Figure 1 (Click for full image)
Figure 1 (Click for full image)
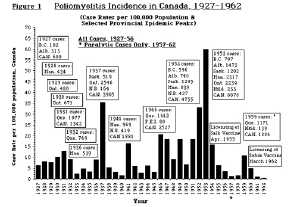
The evolution of a government-focused Canadian response to epidemic polio began in 1927-28 when the first major epidemics hit western Canada and provincial governments, especially in Alberta, responded aggressively (for Canadian incidence data see Figure 1 and Table 1, Table 2 and Table 3). In most provinces, and to varying degrees, provincial polio strategies expanded during serious epidemics with the development of specific preventive, treatment and hospitalization services that were freely available to all polio cases, regardless of income. No other disease generated such a broad and unconditional response from Canadian governments during this period -- and with the blessing and cooperation of the medical profession. In the absence of any effective treatments for polio, the assumption of responsibility by provincial governments helped to relieve some of the extraordinary frustrations and pressures polio increasingly placed on private physicians. Bearing the brunt of Canada’s worst epidemics, Alberta, Ontario, Manitoba and Saskatchewan developed the most sophisticated and generous polio policies in this period.
Underlying and reinforcing this Canadian response to the polio problem were several distinctive public health and political factors. Most significant were the close institutional and personal links between leaders in local, provincial, and federal health departments, in the medical profession, and in public health education, research and the centralized, non-commercial production of biological products -- all through the University of Toronto’s Connaught Laboratories and the School of Hygiene. In the first half of the century, these two intimately linked institutions, under the leadership of Dr. Robert D. Defries (1889-1975), stood at the centre of Canada’s public health network and the evolution of Canada’s scientific, political and public health response to polio. Most provincial and federal deputy ministers of health were trained at the School of Hygiene, and thus shared a common professional education and active public health vision disseminated through Defries and Connaught’s founder, Dr. John G. FitzGerald (1882-1940); as well, Connaught’s comprehensive polio research efforts after 1947 proved essential to the development and large-scale production of the Salk vaccine.(11) In many ways, between 1914 and mid-1930s, these close relationships played a similar role in the Canadian management of diphtheria, a dangerous and much-feared childhood disease that shared several features with polio until an effective immunizing toxoid was widely tested and freely used by the early 1930s -- largely through Connaught’s and the Ontario government’s pioneering leadership.(12)
The establishment and expansion of provincial polio programs closely followed conjunctions between major epidemics in Canada and the emergence of new polio therapies on which public hopes and dramatic publicity focused, and often despite medical controversy over their effectiveness. Striking conjunctions occurred in 1927-28, 1936-37, 1941-42, 1952-53, 1953-54 and 1959-60. Each involved different polio treatments, ranging from a human immune, or convalescent serum, in the late 1920s and early 1930s, to prophylactic nasal sprays in the mid 1930s, to the unorthodox physical therapy methods of Sister Elizabeth Kenny in the 1940s, to gamma globulin in 1952-53, and finally to two different polio vaccines in the mid 1950s and early 1960s. The enthusiasm surrounding these "polio weapons" largely originated in the United States and created significant political pressures north of the border for their expedited use. In an effort to appear to be doing something against the ravages of polio, most provincial governments, and eventually Ottawa, assumed direct control of the financing and production of such therapies and distributed them freely and unconditionally.
The severity of Canada’s second epidemic wave, which peaked in 1937, brought the medical, public health, technological and political pressures of polio in Canada to a dramatic new level. This second wave involved two major provincial epidemics: Manitoba in 1936, and Ontario in 1937. The management of the Ontario epidemic by the provincial government marked the most comprehensive and unconditional preventive, treatment, hospitalization and after-care program yet deployed against any infectious disease in Canada. Each of these aspects of the 1937 Ontario epidemic will be discussed below.
Nationally, the seriousness of the 1937 Ontario polio epidemic helped focus the attention of the Ontario Department of Health and other Canadian public health authorities on an central question: Just how far should any government be compelled to go to ensure the advantages of modern treatment for its people? The Ontario government’s high level of financial involvement in polio treatment and after-care support during and after this epidemic reinforced the growing value of "state medicine," and set important precedents in its subsequent expansion, especially in the face of worsening polio epidemics in the 1940s and 1950s across Canada.
Second Wave Epidemics and the Provincial Public Health Response
After the rise and fall of the first epidemic wave that, in turn, hit British Columbia and Alberta in 1927, Manitoba in 1928, Ontario in 1929 and 1930, and Quebec in 1931 and 1932, during the "polio seasons" of 1933 and 1934 Canadian polio incidence remained low. Alberta was hardest hit in 1935, while in 1936 the disease was confined mainly to Manitoba. However, in 1937 alarming epidemics struck Alberta, Manitoba, New Brunswick, Saskatchewan, and most severely in Ontario. Nationally, 1937 was the second worst polio year in Canadian history with a reported case notification rate of 35.4 per 100,000, representing some 4,000 cases and 200 deaths across the country. Only 1953 was worse when a national case rate of 60 was reached, the highest national polio case rate ever recorded in North America, and among the highest in the world.(13) The majority of the 1937 cases occurred in Ontario, although the seriousness of the Alberta and Saskatchewan situations provoked similar provincial responses (see Figure 1 and Table 1, Table 2 and Table 3).
During the summer and fall of 1936 paralytic poliomyelitis was a "disease of outstanding importance" in Manitoba, and was worse than the epidemic of 1928, when 434 cases and 37 deaths were reported. Then, according to a prominent doctor, the disease incited "a terror" in Winnipeg comparable to the air raids of World War I.(14) In 1936, a total of 525 cases and 37 deaths were reported across the province, with most rural areas involved.(15) One major difference from 1928 was that the Manitoba Department of Health and Public Welfare was under the leadership of a new Deputy Minister, Dr. Fred W. Jackson, who held a Diploma of Public Health (D.P.H., 1929) from the University of Toronto School of Hygiene.(16) He assumed a much broader and more direct role in the management of the epidemic in terms of strict disease control measures, diagnosis, prophylaxis and after care. By contrast, the 1928 epidemic was managed largely through the use of convalescent serum under the direction of a University of Manitoba Research Committee with the financial support of the provincial health department.(17) Convalescent serum, an immune serum prepared from the blood of recovered polio cases, was the great medical, popular and government hope of Canada?s first wave of epidemic polio. Despite increasing and largely American scientific controversy surrounding the serum?s real value in minimizing paralysis, most provincial governments prepared and supplied it free to all diagnosed polio cases starting in 1928.(18)
In 1936, under Jackson’ direction, Manitoba’s provincial health department implemented a broader approach against polio. An epidemiologist was appointed to work in the hardest hit area of Boissevain. He was given the "power to insist on rigid observance of quarantine regulations" and act as a diagnostic consultant for the affected area. As the situation deteriorated more special investigators were appointed to expand these services across the province. Public Health Nurses were also assigned for an intensive education program to urge parents to call a doctor quickly in the event of symptoms of the disease appearing. Some municipal governments passed local by-laws to prevent "the ingress of individuals from the infected areas." Despite such strict measures, Jackson felt they "do not seem to be of great value, at least such would appear to be the case."(19)
Despite the debate about its value, convalescent serum remained central to the Manitoba government’s polio strategy. The medical community, and especially the public, demanded that the serum be used, "whether or not [it] is of value...."(20) However, early in the epidemic, physicians remained overly dependent upon spinal tap confirmation before giving the serum. With no simple diagnostic test available for polio comparable to the diphtheria schick test, the only diagnostic method was the lumbar puncture, or spinal tap. An examination of the spinal fluid for characteristic cell counts indicated polio, although this was often done after the appearance of paralysis. Waiting for a spinal tap often led to "disastrous results" and Jackson stressed to doctors that a clinical diagnosis alone was enough to justify immediate serum administration, even though until weakness or paralysis was evident, the clinical symptoms of polio were difficult to differentiate from many other common childhood ailments. Further bolstering confidence in the serum, however, many physicians claimed that the general clinical results obtained from it were "quite comparable to those secured when diphtheria antitoxin is given in a case of diphtheria."(21)
The most significant problem Jackson’s
Department faced in managing the 1936 epidemic was its severity in the
"dried-out area[s]" of the province in the midst of the Depression. Many
parents delayed or refused to call a doctor simply because they could not
afford to pay for their services. As the serum’s effectiveness was thought
to depend upon its early administration, if parents could not afford to
see a doctor, it became "very apparent that something had to be done to
ensure that everyone in the district who became ill had medical attention
at the earliest possible moment."(22) Through Jackson’s personal efforts,
the local governments of each of the affected areas were convinced to provide
free diagnostic and treatment facilities unconditionally to every resident,
with the municipality paying the doctor’s fee. Physicians were paid a special
scale of fees which was about two-thirds the normal charge. Special resolutions
were passed by local governments to offer and also widely advertise this
service. The municipal by-law read:
The 1937 Ontario "infantile paralysis" epidemic recorded a total of 2,546 cases, at a case rate of 70 per 100,000, and claimed 119 lives. Of this total, 758 cases and 31 deaths were registered in the City of Toronto (population 648,309) at a case rate of 117.(26) Since the majority of cases occurred among children under 10 years of age, the age-specific incidence rate in this group in Toronto was 510. Just over half of the number of provincial cases exhibited paralytic symptoms, and by the following March, 839 remained paralyzed to varying degrees.The size, severity and dramatic intensity of this epidemic came as a major shock to Ontario. Such an epidemic situation has not been repeated in the province by polio or any other infectious disease.(27)
As had been the case in 1929, an epidemic in 1937 was not unexpected because it followed Manitoba’s in 1936. Using the general Canadian trend of epidemics moving from west to east since 1927, and an apparent seven year epidemic cycle, the Ontario Society for Crippled Children (OSCC)(28) predicted a significant outbreak in 1937 and devoted the entire June issue of its newsmagazine, The Horizon, to articles on polio.(29) This striking geographic and epidemiological pattern can be explained by the relative regional differences in immunity levels to the three distinct types of the poliovirus. In Canada this situation shifted from west to east through the first decades of the twentieth century with the establishment of new and isolated settlements, particularly in the west and northern regions, along with rising population levels, improving health and economic standards and increased personal mobility through the growing use of automobiles and air travel.
The Horizon issue included articles by the Minister of Health, Dr. J. A. Faulkner, his Chief Medical Officer of Health, Dr. J.T. Phair, and the Director of Preventable Diseases, Dr. A.I. McKay. The tone of these and other articles emphasized the public health value of "the most rigid quarantine," and the continuing use of convalescent serum. McKay was well aware of the serum debate, but argued that "Even ten children escaping paralysis as the result of the use of the serum certainly warrants any effort in time and money expended in making it readily available."(30)
When the epidemic began, the press coverage of the serum was as hopeful as ever, but as it quickly escalated, clear and public signs of controversy became evident among physicians and local health officials over its value.(31) Such unusually open debate went beyond the serum issue itself, with some doctors publicly questioning the seriousness of the epidemic itself.(32) The serum policy outlined by the Minister of Health to every Ontario physician stressed that "The serum has no value as a preventive agent and should not be used except for the treatment of children showing the early signs of the disease."(33) When the serum was given, such cases were required to be treated as official polio cases and thereafter were subject to provincial and local health regulations.(34) Later they were also eligible for free diagnosis, treatment and hospitalized after-care for a limited period. Once diagnosed, provincial health regulations required isolation of the patient for three weeks and all family contacts quarantined; "rigid adherence to the regulations" was required.(35)
Early in the epidemic, local medical officers of health (MOHs) requested special diagnostic consultants from the province. Thirteen full-time physicians were appointed and given a three-day course on polio’s epidemiology, diagnosis and the early treatment of paralyzed cases. They were each assigned a specific region and by August a total of sixteen consultants provided much needed clinical assistance to MOHs province-wide. They also gathered considerable statistical and other types of information which were later used in the most detailed report ever published on a Canadian polio epidemic.(36)
With three major daily newspapers in Toronto, in an era when the public relied on newspapers for the majority of their news,(37) the emerging polio epidemic was a big story by mid-August. The provincial health department was determined to provide an extensive public education program about the disease and was confident that it could control how the press covered the epidemic. Carrying out both efforts soon proved difficult, if not impossible. In early August, the Toronto Board of Control, fearing the economic impact of the epidemic on city business and trade, instructed the Toronto Board of Health to limit public information and statistics on the outbreak. Within a day, however, Toronto MOH, Dr. Gordon Jackson, was forced to lift the ban.(38) Provincial health authorities were disturbed by the controversy and assured the public that there would "be no putting the lid on" information about the current epidemic.(39) In the Department’s effort to keep the public informed, "the newspaper publicity was changed to suit the peculiarities of the editors." A detailed full-page "Statement by the Ontario Department of Health on POLIOMYELITIS ("INFANTILE PARALYSIS")" was placed in all daily papers in the province by 30 August.(40) The Department also held daily press conferences during the peak weeks of the epidemic to insure "that accurate information would be available to the public at all times."(41)
The local management of the epidemic in Toronto was the focus of further controversies over the delaying of school openings, the closing of public pools, parks and churches, and whether or not to cancel "Children’s Day" at the Canadian National Exhibition (CNE). The issue of postponing public school openings beyond Labour Day to minimize contact among children developed into an emotional debate between health authorities and physicians inside and outside the city.(42) As had been the case in Alberta during the 1927 epidemic, and elsewhere, this debate highlighted the uncertainty within the medical community between the conflicting neurotropic and systemic models of the disease.(43)
By the early 1930s, and since the
1910s, the dominant scientific model of poliomyelitis was that the poliovirus
was completely neurotropic; i.e. present and pathogenic only in nervous
tissues as demonstrated experimentally in laboratory monkeys. This model
focused on the specific paralytic pathology of the disease with limited
attention devoted to its general clinical course or natural epidemiology.(44)
However, this laboratory model of polio had little practical value for
many physicians, many of whom could not reconcile the acute polio symptoms
they saw in their patients with the idea that only the nervous system was
involved. Another, broader understanding of polio had emerged at the turn
of the century, based on pioneering epidemiological and clinical work in
Sweden that had established the concept that polio was a generalized systemic
infection with paralysis "but an accidental and incidental occurrence."(45)
This inconsistency remained a strong undercurrent which increasingly surfaced
to challenge the orthodox neurotropic model as North American epidemics
grew larger during the 1930s. For example, a report on a 1935 epidemic
in Virginia concluded:
This issue first arose in Toronto Board of Education with a motion officially asking parents to at least keep their children at home during the CNE.(49) The motion failed, but the issue was taken up by Dr. R.H. Saunders of the Toronto Board of Health. Saunders suggested that Children’s Day alone should be canceled, since schools, public parks, pools, theatres and churches had already been closed to children during the epidemic. The Board of Health had been vociferous in its pleas for parents to keep their children at home, and it seemed that to be consistent, 200,000 children should not be encouraged to mingle freely at the CNE on Children’s Day.(50) The 1937 edition of the CNE was expected to be large, particularly to celebrate the Coronation Year of King George VI. Also, the local economy had recently improved and an extensive international advertising campaign had been launched to attract the largest crowds possible.(51) The epidemic had forced the closure or postponement of smaller local fairs across the province, but any thoughts of doing the same with the CNE were vigorously resisted by CNE and city officials. Toronto’s mayor attacked the idea and denounced its supporters as "unfit representatives of the public." This left MOH Jackson in a difficult position in advising parents to keep their children at home and had to admit that he had no power to compel them to do so.(52)
Children’s Day went on as scheduled, the CNE actually doing very little to meet concerns about the epidemic other than canceling its annual Baby Show Contest and offering free tickets to children good for the duration of the fair.(53) Nevertheless, parental concerns and the extensive publicity about "paralysis" had the effect of keeping attendance for the day down 78,000 less than the previous year, and reduced by 300,000 over the entire 1937 run of the CNE.(54) The local press, reliant upon considerable advertising revenues derived from the CNE directly and indirectly, tried to maintain a positive outlook, although there were differences evident in how each paper covered the issue.(55)
This controversy and intense press attention reflected the confused medical and scientific understanding of polio, the frustrating lack of progress in developing effective measures to prevent and control epidemics, and the profound fear "paralysis" generated among parents and the community. Mothers felt this fear and frustration the strongest and their voices were frequently heard in the daily press in painful letters to the editor and through many poignant human interest stories.(56) One front page story published in the Toronto Star at the peak of the epidemic dramatically captured this situation. The headline read, "Mothers of the World Again Must Bear Brunt in War With Paralysis," the article couching maternal fears in war imagery. "All we can do is wait until the enemy cracks us down. Then we play stretcher bearers. Just carrying off the stricken." Although it attempted to ease parent’s anxieties about the disease, the article admitted that "the truth unquestionably is that after 57 years, medical science is totally in the dark" on how infantile paralysis originated, was transmitted, and how valuable convalescent serum really was. Indeed, in this war, "the front line troops are not the scientists of the world, but the mothers of the world."(57)
PREVENTION AND TREATMENT METHODS IN CANADA
"Paralysis Nose Spray: Just Squirt and Smile"(58)
During the polio season of 1936 widespread enthusiasm developed around the prophylactic potential of nasal sprays based on the prevailing idea that the portal of entry of the poliovirus was the olfactory nerves of the nose.(59) Interest in the chemical blockade of the nasal mucosa first emerged in 1934 with attempts to protect white mice against an intranasal inoculation of equine encephalitis virus with a tannic acid solution.(60) Similar experiments were conducted with as many as 150 different solutions on mice using the St. Louis type of encephalitis as a "feeler" for polio research with monkeys.(61) A picric acid solution was eventually settled on, and in the summer of 1936, Dr. Charles Armstrong of the U.S. Public Health Service advocated that such a spray be given a human field trial based on monkey experiments and the repeated spraying of himself "and a small group of volunteers without apparent ill effects." That summer a serious polio epidemic in Alabama presented an opportunity for such a field trial.(62) Federal and state health officials had hoped it "would be a test by and under the [medical] profession," but it soon became, "largely through the activity of the people themselves..., a test by the masses, largely uninstructed, with all the many variations of method which such a procedure implies."(63) The U.S.P.H.S. issued a statement on the nasal spray which stressed that "homemade concoctions are not favored." Also, "early applications at least should be administered by a physician." This statement was published in the Manitoba Medical Association Review in September 1936 during the peak of the province’s polio epidemic.(64)
The U.S. statement had essentially given permission to Manitoba physicians to try using the spray. Its use was also encouraged by Public Health Nurses who had been sent to the affected areas by the provincial department of health to "[give] instruction where requested, on the use of the nasal spray."(65) However, the Manitoba government did not seem to pay serious attention to the spray and made no attempt to control its use or evaluate its effectiveness. The members of the Dominion Council of Health, Ottawa’s national health advisory committee made up of the federal and provincial deputy ministers of health, plus others, including the Director of Connaught Laboratories and the School of Hygiene, echoed concerns that only physicians administer the spray; otherwise the topic generated little discussion.(66) This relative complacency in Canada lasted until the inconclusive results of the Alabama trial were published in early 1937.
Controlled field trials of prophylactics were rare prior to the late 1930s, with random selection of control groups rarely done systematically.(67) Generally, however, it was not until after 1940 that "[t]he concept of randomization gradually gained acceptance in clinical medicine..."(68) One of the first such field trials took place ten years earlier in Ontario with diphtheria toxoid. Diphtheria toxoid, prepared from diphtheria toxin inactivated with formaldehyde, had been discovered in 1923 by Gaston Ramon of the Pasteur Institute in Paris and was quickly applied in Canada through a close relationship between Ramon and Dr. J.G. FitzGerald, Director of Connaught Laboratories and the School of Hygiene. Of particular significance in expediting its use in Canada, and later in the United States, was the development at Connaught of a diphtheria "reaction test" by Dr. P.J. Moloney, which became known as the "Moloney Test." By October 1925 the new toxoid was ready to be given to children in Canada, with initial studies focused in Hamilton, Brantford and Windsor. This was followed by an unprecedented scientific, statistical and public health attack on diphtheria in Toronto involving 36,000 children between 1926 and 1930. The study conclusively proved that the toxoid reduced diphtheria incidence by at least 90% among those given three doses. This work represented the first statistical demonstration of the value of a non-living vaccine in preventing a specific disease. Subsequently, diphtheria incidence declined sharply in Canada, dropping effectively to zero cases and zero deaths in many centres by the early 1930s.(69)
The most significant problem noted in the 1836 Alabama nasal spray trial seemed to be technical, with the spray not reaching high enough into the nose to be effective. A long special tip was thus needed on the atomizer which could only be inserted by a professional nose-and-throat specialist. Furthermore, experiments using a zinc sulphate spray on monkeys reported in June 1937 suggested that this was more effective than the picric acid spray and was worthy of a human trial.(70)
In Ontario, parents grew desperate for any kind of preventive measure as the 1937 epidemic spread and news of the potential value of the nasal spray generated increasing demands that it be given by private physicians. Such demands were stimulated by widely-quoted press statements from American spray enthusiasts, such as noted virologist Dr. Thomas Rivers. In August 1937 he recommended: "If I had a child in an area where poliomyelitis appeared, I would take my child to a good otolaryngologist and ask him to apply the spray in the manner set forth by Dr. [Max] Peet," who had developed the newer treatment.(71) Despite the caution of some MOHs, doctors began offering the spray and considered it "both safe and cheap." A London, Ontario doctor provided the press with the spray’s formula and application procedure. Newspapers quickly picked up the spray story and even reported that some desperate parents were spraying their children’s noses with salt water. Other physicians were not so sure about the spray, one warning that "until we have definite proof that children contract the disease through the nose," there was "no point in using the spray, which [was] difficult to administer, uncomfortable and possibly dangerous." Despite such controversy, physicians were soon overwhelmed with calls from parents wanting the children treated with the spray.(72)
The Ontario government thus came under intense pressure to provide the spray, but did not know if it would work or if it was safe. In order to prevent an "epidemic of spraying,"(73)and more importantly, to be able to offer a definitive opinion about the spray’s preventive value, the province gave approval for a plan to carry out a nasal spray field trial. This was limited to 5,000 Toronto children, in addition to an observed control group of equivalent size. The control group was obtained by Public Health Nurses who canvassed each of Toronto’s eight health districts, which seemed to provide "a reasonably representative group."(74) This plan was designed to avoid the pitfalls of the Alabama trial, since it was clear that "unless great care is exercised, no really helpful information will be likely to come out of such further work."(75)
The Ontario plan was immediately presented to a group of Toronto otolaryngologists from the city’s hospitals, who would administer the spray in special clinics.(76) The trial was financed entirely by the province and carried out with the assistance of the Toronto Department of Health. Responsibility for the study was assumed by the Hospital for Sick Children and the School of Hygiene, with the entire trial under the supervision of Dr. R.D. Defries, Acting Director of the School and Connaught. As was noted after the trial, "In few cities has there been such whole-hearted co-operation on the part of the administrative authorities, the public, and the press in an undertaking which was definitely presented as an experiment. To this extent the study was unique."(77)
The trial was first publicly announced in the Toronto press on 30 August, its details outlined with "a very conservative statement" that emphasized the limited size of the "experiment" and included a consent form for interested parents to return. A chance to participate in such a hopeful experiment generated intense public and media interest and within three days more than 6,000 forms flooded in from parents who clamored for any kind of protection for their children.(78) Those who could not be included in the "experiment" demanded the spray from their doctors.(79) The first clinics opened on 31 August with 5,233 children sprayed by 5 September, and 4,585 children sprayed a second time two weeks later.
The trial organizers were concerned about how well the public would respond, particularly since parents had been strongly advised to keep their children away from crowds. The large response was surprising and attributed "in no small measure, to the excellent publicity given to the study by the press who, through suitable articles and news items, kept the public informed of the purpose and progress of the effort." The experimental nature of the trial was stressed in the press, "although some measure of hope was offered,"(80) thus effectively raising public expectations and demand for the spray, either within the formal structure of the trial, or on the free market. As was stressed in newspaper coverage of the trial, here then was a clear chance for children and their parents to take part in an important scientific experiment.(81) But such publicity made it difficult to limit the spray’s use and prevent other communities, and even some private businesses, from making the spray available to its citizens or employees.(82)
As was reported in November 1937, the trial clearly demonstrated that the spray was ineffective as a polio preventive, and also potentially dangerous to those treated. Eleven cases of polio were reported among those sprayed, while nineteen cases occurred in the control group, suggesting that the differences between the attack rates in each group were not statistically significant.(83) As was the case with the 1936 Alabama trial, the Toronto report blamed faulty administration methods for the failure of the spray. The objective of the nasal spray was to block the poliovirus from entering the olfactory nerve, and thus a temporary loss of the sense of smell (anosmia) was expected. When this was tested during and after the trial, no more than 25 per cent of the children sprayed reported losing it.(84) Most devastating, however, it was found that among those children losing their sense of smell and/ or taste soon after the trial, many had not regained it months later. There was also a notable case of anosmia among one of the trial organizers, Dr. Donald T. Fraser, who would not try anything on anybody that he would not try on himself. He took this self-experimentation in stride, though, noting later "that his only objection to this loss was that he couldn’t enjoy his sherry anymore."(85) As well, the practical problems of organizing, deploying and administering the spray quickly and safely during the emergency of an epidemic largely undermined enthusiasm for its further scientific study or use.(86)
Despite its lack of success, the Toronto field trial marked an important step in polio research with its relatively high standards of professionalism, methodology and administrative and public cooperation. This was reinforced by the close physical proximity between the provincial health department, the Hospital for Sick Children and the University of Toronto’s School of Hygiene and Connaught Laboratories, along with the experience of, and close professional, academic and personal links between Defries and the others involved. These were features lacking with the earlier use of the spray in Manitoba, and especially in Alabama, and with other prophylactics used against polio, such as convalescent serum and the two rival polio vaccines developed by Brodie and Kolmer in 1934-35. These were primitive "killed" and "attenuated" precursors to the Salk and Sabin vaccines, and under the pressures of major polio epidemics, as well as scientific and commercial rivalry, were widely and prematurely used in the U.S. with considerable controversy and some tragic results.(87) In the wake of the Toronto nasal spray trial it also became clear that "the problem of preventing human poliomyelitis was not to be easily solved on the basis of evidence deduced from the experimental disease in the rhesus monkey." Combined with other evidence, polio historian Dr. John R. Paul argues that "the experience in Toronto aroused uneasiness about the whole hypothesis of a nasal portal of entry in man."(88) Indeed, soon after the Toronto trial, success was quietly reported in the long standing problem of isolating the poliovirus from human intestinal washings, results which were highly significant for later epidemiological and immunological research.(89)
One of the most serious and unexpected developments of the 1937 epidemic was the large number of "bulbar" cases of respiratory and/or throat paralysis, which impaired breathing and swallowing and usually caused death.(91) Polio mortality statistics averaged about four percent of reported cases, but the management of bulbar cases represented a major medical and technological challenge. The image of the "iron lung" was first ingrained into the Canadian public consciousness during the 1937 Ontario polio epidemic.
The first "iron lung" or electric tank respirator designed for severe polio cases was built in 1928 at Harvard University by Philip Drinker.(92) It was essentially a metal tank into which all but the head of an individual was sealed. A motor, or hand crank, operated a set of bellows, and since the head remained outside of the lung, the negative pressure inside acted like the human diaphragm and forced the lungs to expand and contract to allow regular breathing. The first iron lung in Canada was an original Drinker model that arrived at Toronto’s Hospital for Sick Children (HSC) in 1930, and it apparently remained the only one in the country until August 1937.(93) Bulbar cases were rarely mentioned during earlier epidemics since most died tragically when there was little that could be done to help them. Death rates from polio varied widely, between about 4 and 30%, and "tend[ed] to vary inversely with the number of cases, being relatively low in epidemic years and relatively high in non-epidemic years"(94) (Table 3).
The Toronto press focused considerable attention on the need for more life-saving iron lungs as the 1937 epidemic worsened through August. The emergency was leaving "little tots struggling for breath" in hospitals.(95) HSC’s single Drinker machine was used for a small number of mild chest paralysis cases, but on 21 August, a young girl in critical condition was placed in the lung, which happened to be open, but it was clear that she would have to remain in it for a long time. She would then have to be "weaned" off the iron lung when evidence of recovery was clear and periods outside the iron lung could then be progressively lengthened. This situation greatly concerned HSC’s Superintendent, Joseph H.W. Bower. The City of Toronto had ordered one commercial machine for Riverdale Isolation Hospital. London and Hamilton had also ordered lungs. Yet it would be several days at least before Riverdale’s lung arrived, and it would be ten days to two weeks before another one would be available.(96)With this news, Bower knew he would have to build respirators at the hospital for any bulbar cases that might develop.
Meanwhile a four-year-old boy had been admitted with chest paralysis on the morning of 26 August. As the Drinker machine was in use, an experimental respirator for premature infants was modified and coupled with a quickly-built wooden box in which the little boy was placed and stabilized. This "emergency-made ‘lumber lung’" "saved" the child’s life. The boy’s mother then turned to the newspapers to plead for the "wealthy to buy iron lungs," each of which was worth some $2,000. The prominent place of this appeal in the Toronto press reflected the unusual vulnerability to polio among the well-to-do, whose wealth could not protect them from this disease. Two more commercial "lungs" were eventually bought, largely through an "Anonymous Donor."(97) Meanwhile, at HSC, efforts were concentrated on building more lungs. By noon of 27 August, plans were complete and enough parts were ordered and delivered by the next evening to start assembling the first iron lung. Two days later this first lung was complete and placed on HSC’s Infectious Floor; within fifteen minutes a patient was placed in it. By 31 August, four "homemade" iron lungs had been assembled in the hospital’s basement.(98)
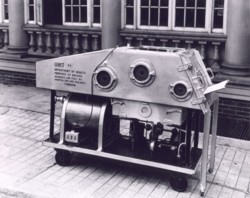 Figure 2 (Click for full image)
Figure 2 (Click for full image)
The Deputy Minister of Health was impressed with the speed of HSC’s iron lung production. Just as the first four "welded steel" lungs were completed the Department ordered three more for use by the province, and shortly increased this order to twelve. With production running 24-hours-a-day, they were delivered within the next seven days. Financed by the province at a cost of between $650 to $700 each, HSC assembled 27 iron lungs under the close direction of Superintendent Bower, who lived in the hospital for the duration of the epidemic (see Figure 2). Most of these lungs were used at HSC or at neighboring Toronto General Hospital, while the rest were shipped to other hospitals in the province, as well as to Winnipeg, Regina and Edmonton. The original "wooden lung" by this time was no longer in use; in response to an emergency call, the Toronto Star arranged to fly it to Denver, thus saving the life of a young girl.(99)
The dramatic story of the "Herculean efforts" at HSC to manufacture iron lungs drew intense press attention. Soon there were riveting stories in the Toronto press describing how "Seven Tiny Heads in a Row Tell of Fight With Disease: Big Steel Monsters Hold Children Battling Bravely to Overcome Paralysis of Lungs." A month later another story detailed the way "Massive Iron Lungs Grotesque, Glorious, Coax Life to Tots: Hushed Rhythmic Action Keeps 7 Tots Alive in Hospital Room: In Gleaming Row."(100) Over the years the press covered the birthdays and even the weddings of "famous" polio sufferers who had been confined to iron lungs indefinitely.(101)
Despite the many stories of lives being saved by wooden or iron lungs, their efficacy in preventing bulbar polio deaths remained controversial. During the 1937 epidemic, 63 polio cases were treated in iron lungs, and by the following March, 40 had died, 12 had recovered and 11 still remained in respirators, six of whom "will probably continue to require the respirator indefinitely."(102) Despite this generally grim record, iron lungs had a significant effect on public perceptions, ranging from fascination with the hopeful power of science and technology in an otherwise fruitless war with polio, to terror, as rows of iron lungs encased polio’s helpless young victims for weeks, months or years. The iron lung symbolized the disease and its worst possible effects while at the same time it provided the medical community with a specific and hopeful technological tool against them. Still, the limited supply and success of iron lungs, especially during the crisis of an epidemic, frequently raised the difficult ethical dilemma of having to decide who to treat and for how long. Nevertheless, the iron lung also gave the provincial government another opportunity to demonstrate that it was doing everything possible against the worst effects of this disease.
Other than the efforts of Alberta
in 1927-28, where a special polio hospital was opened in Edmonton,(103)
the issue of treatment, hospitalization and after care of paralytic polio
cases was rarely addressed by provincial governments for the next decade.
In the wake of the 1936 Manitoba epidemic the province took a modest step
forward in how it viewed the problem of after-care and hired an orthopaedic
specialist, Dr. A.A. Murray, who at no charge, assessed every paralytic
case outside of the Greater Winnipeg area, and outlined the required treatment
methods to minimize deformities. This service was recognized as "a new
departure in the Public Health work of Canada."(104) The issue of hospitalization,
however, was rarely mentioned, and was viewed as a last resort for orthopaedic
surgery. But as Murray stressed, patients "should be discharged to their
homes as soon as they feel well following operation, and so save an enormous
amount of public money." He once felt that the state should freely provide
splints, appliances and hospital and medical care to the indigent, but
his polio work seemed to change his mind. Few such patients took care of
free appliances and he thought they were "apt to lose their independence
and capitalize on their disability in order to live without work."(105)
These conservative views, likely hardened by the Depression, were not shared
by such provincial health authorities as Deputy Health Minister Jackson,
whose public health background and recent experience during the epidemic
reinforced a more liberal approach. He argued that since
In mid-September, at the request
of the province, the OSCC called a meeting of orthopaedic surgeons in Toronto.
Based on conclusions reached at the earlier symposium, Dr. D.E. Robertson,
Chief Surgeon and orthopaedic specialist at the Hospital for Sick Children,
recommended that:
 Figure 3 (Click for full image)
Figure 3 (Click for full image)
At the meeting of orthopaedic surgeons, the province agreed to an aggressive plan to provide standardized frames and splints "without delay for all cases showing evidence of paralysis or muscle weakness."(114) These appliances were manufactured at the government’s expense at HSC, and at Hamilton General Hospital and London’s Victoria Hospital, and were distributed by the Department, free of charge, to all paralysis cases.(115) This was the first time that standardized splints and frames had been prepared for polio treatment in North America. Previously they had been made to order, which took days or weeks, but under this system, when an order arrived giving the size, height, length of leg, or arm, "the frames and splints are on their way in a few minutes."(116) By late November, with some 2,531 cases reported in the province, a total of nearly 2,000 splints and frames had been provided free by the Ontario government.(117) These splints soon became known as "Toronto splints" and until the early 1940s were the North American standard. In 1939 the National Foundation for Infantile Paralysis began stockpiling as many as 15,000 of them in New York City, "ready to be flown wherever doctors demanded them."(118)
The provincial department went further
in their polio policy and recognized that "deformity arises from too early
attempts to get around, from unsupervised treatment or from no treatment
at all." The Ontario government therefore decided on 16 September,
The principal purpose of the "Ontario Orthopaedic Hospital" and the orthopaedic wards in the other designated hospitals, was also to teach patients and their parents how to manage the effects of "paralysis" at home. During two days in October they were "personally advised and lectured as to the paramount importance of keeping the little patients on the frames and in the splints." Otherwise, parents were barred from seeing their children, except through glass, while nurses and doctors gave the patients "weeks of routine, to accustom them and to discipline them, to the steep road that lies before them."(123)Parents were instructed to carefully massage the weakened limbs, turn the child regularly and watch for redness of the skin. They were to occupy their child’s mind, but warned not to "call attention to his condition, don’t pamper him, don’t tire him, keep the house quiet, give him plenty of rest and sleep, etc."(124) For many parents, such a regimen was very difficult, if not impossible, and in many cases had to continue indefinitely.
Some parents had difficulty believing in or accepting the prescription of long term immobility which prevailed in Canada until 1941-42.(125) This view was evident from a series of historical questionnaires distributed to polio survivors across Canada.(126) Recovery was "too slow" for many because they believed immobilization "caused a great deal of muscle atrophy."(127) Among polio survivors, this type of treatment seemed insensitive and often led to dissatisfaction, if not rebellion against medical authority. Objectification was common. One survivor has vivid memories of feeling like "a prisoner" in the hospital and being "tied to my bed" on a Bradford Frame with a straight-jacket. "No one treated me like a person."(128) Frustrated by such treatment, osteopaths were sometimes resorted to, as were chiropractors, much to the chagrin of physicians during much of the epidemic era.(129) In one 1937 case, "we had an osteopath coming in one door while the medical man was going out the other." A watch was kept in case the doctor returned, in which case "we’d quickly put the irons back on."(130) This flouting of medical authority left some paralyzed children confined at home without any medical attention. This happened to a 14 year-old boy whose parents constantly turned him over and over again in bed. Fifty years later he vividly remembered how "he would scream and scream" in pain.(131) Parents were nevertheless repeatedly warned "against the bad advice of well-meaning but ignorant relatives and friends and irregular practitioners."(132)
One particular irregular practitioner who worried Ontario doctors was Sister Elizabeth Kenny, an unorthodox Australian nurse. In the late 1930s she had become a kind of cult heroine based on press reports of her "miraculous" work for polio patients in Australia and her resultant clashes with orthopaedic surgeons and physicians. The Canadian popularity of Sister Kenny and her methods of active massage and heat, preceded her personal arrival and medical acceptance in North America in the early 1940s.(133) Sharp conflicts frequently occurred between parents and physicians when her methods were applied in the home.(134) In one case in 1939 the mother of a two-year-old boy "asked the surgeon whether the Sister Kenny approach might be beneficial. He ridiculed her and made her cry -- his approach was the only one!"(135) Others stricken with polio during the late 1930s felt that "the Kenny Method should have been used on me right from the first, then I wouldn’t be so disabled today."(136)
One of the more vexatious clashes over the Kenny methods took place in Toronto during the 1937 epidemic. A ten-year-old child suffering from almost total paralysis lay at the centre of a battle between her mother, described as a "practical nurse," her family physician, the Hospital for Sick Children, and the provincial health department. The conflict was driven by the mother’s "stubborn" insistence on nursing her daughter at home using the "non-restrictive" methods she had read about that were being advocated by Sister Kenny. Sparking what became a year-long struggle was the mother being "forced" to take her daughter to HSC to confirm the polio diagnosis by spinal tap. According to her daughter, "My mother refused to let them admit me and we waited there for hours before they let me go." While at home "My parents let me do whatever I felt I could do, even if I fell or hurt myself." However, this clash cost her family financial assistance from the province.(137) Benefits were contingent on cooperating with the standardized system set up by the government. By contrast, the father of a nineteen-year-old woman also stricken with polio in 1937, who borrowed from his life insurance to pay the hospital bill, was surprised the following spring to receive a government cheque that "reimbursed him for the hospital bill, which included special nurses."(138)
The Ontario Society for Crippled Children cooperated closely with the provincial government’s hospitalization and treatment plan with transportation and follow-up services. It also loaned one of its staff to the new polio hospital, who served as a link between the Department of Health, the OSCC and other local service clubs throughout the province.(139) The OSCC executive was concerned, however, that many families might be unaware, unable, or even unwilling to take advantage of the appliances and hospitalization offered by the government. Families needed to be "worked up to demand these free services, as it is apparent that many physicians will not act promptly, if at all." The Department recognized the need to protect its not insignificant investment and agreed "that a follow-up nursing service will be of the utmost importance in conserving surgical treatment which has been instituted in hospital." The province was "prepared to spend a considerable amount of money in hospitalizing children and providing them with the necessary equipment."(140)
The follow-up nursing program began in early November 1937, the OSCC taking on two extra public health nurses for a year to meet the demands across the province at a total cost of $7,000. To meet these extra costs the OSCC was forced to launch a major fund-raising campaign in December.(141) This program was reliant upon the Department keeping track of each paralytic case by using serum records and outlining to the parents and attending physician of the necessary after-care. If necessary, this information was forwarded to the local MOH.(142) By May 1938, OSCC’s nurses had visited some 800 paralytic cases across the province, with visits continuing for some 500 of these(143)
The visiting nurses were first required to check with the local MOH and each patient’s private physician in order to get permission to visit and assist with each case.(144)While this procedure generally met with cooperation from the medical profession, the zeal of some nurses, and especially the press statements from OSCC’s Reg Hopper, generated conflict with some physicians. Hopper made his concerns public in press statements in December "with respect to the individual patients he had found without proper after-care." To McGhie, the Deputy Minister of Health, such statements were "a little dangerous," and he worried that "physicians who have been responsible may not react kindly."(145)
One such upset physician was none other than Dr. D.E. Robertson, Chief Surgeon of HSC, who was quite "disturbed" about Hopper’s suggestion that the OSCC was responsible for the treatment of convalescent patients. Robertson, who until this point served on OSCC’s Board of Directors, was offended when an OSCC nurse approached him for permission to visit one of his private patients. He refused, and as he explained to McGhie, a "voluntary organization can never do a thing as well as a Government Department such as yours did with the polio epidemic last autumn."(146) However, Hopper was clearly told by the government just what the OSCC’s role was in its follow-up work: 1) continue to uncover unreported cases; 2) gather as much data regarding known cases; and 3) avoid entering the field of treatment. To avoid further embarrassment, all material used for publicity and appeal purposes had to be reviewed by the Department.(147) All this was carefully done without upsetting the Department’s close relationship with the OSCC and their important and useful follow-up program.
While some individual physicians may have been upset with the aggressiveness of the OSCC, this follow-up program and the Ontario government’s overall handling of the epidemic, generally received strong and enthusiastic praise from all who were closely associated with it.(148) Federal health officials in Ottawa were "greatly impressed" with McGhie’s detailed report on the epidemic to the Dominion Council of Health. The Federal Director of Public Health Services, Dr. John J. Heagerty, suggested that "a copy should be sent to the League of Nations for their information," since he felt that the province’s efforts during the epidemic were the "most comprehensive that has ever been undertaken anywhere."(149)
Ontario’s experience with polio in 1937 reinforced a significant shift in the Department of Health’s larger approach to "state medicine." At a December 1938 meeting of the Dominion Council of Health, Ontario’s new Minister of Health, Harold J. Kirby, posed the difficult question, "How far does the responsibility of the Provincial Department of Health go in the treatment of disease?" He reported that recently almost all of his Department’s total budget was "spent on activities that are in the main treatment." It seemed increasingly clear to the Minister there was strong public and professional support for the idea that the government might properly assume responsibility for the expense of the more costly methods of recognized treatment. "Frankly, the therapeutic aspect of the public health program is swamping the prophylactic." His report outlined his government’s expenditures on biologicals and other direct treatment agents, its venereal disease treatment program, cancer treatments, and the costs of hospitalization for polio patients.
In a number of provinces during the mid-1930s, government interest in cancer treatment, in particular, as with polio, was a new extension of provincial health services against prominent and growing public health threats. By 1938 the Ontario government had spent over $750,000 to set up seven provincial cancer clinics, and bought seven grams of radium (worth $400,000 alone). The clinics provided diagnostic and treatment services with radium and x-rays, but were designed "for the indigent and near-indigent groups in our population." The fees were kept as low as possible, "having in mind the fundamental objective of establishing the clinics, namely the provision of modern facilities for cancer treatment accessible to all."(150)
Prior to 1937 the Ontario government spent an average of $4,000 per year on polio, mainly to pay blood donors and to make convalescent serum. However, as Kirby outlined, in 1937 "the interest of the Department in the matter of [polio] treatment was expanded far beyond that ever previously conceived." In total, the government spent $197,000 during the epidemic, "$152,363 of which was for treatment."(151) Yet the widely-acknowledged success of the government’s management of the epidemic left Kirby with a more significant question to consider: "Frankly, how far should any government be compelled to go in ensuring for its people the advantages of modern treatment?"(152) The 1937 epidemic established an important precedent and reinforced a growing trend towards "state medicine." It was clear that polio, despite its relatively minor incidence and mortality compared with cancer, was a disease that, even more than cancer, required that the public be given as much access to the advantages of modern treatment as the state could possibly afford, "regardless of station." In subsequent years, the Ontario government worried about further polio epidemics that might prove even worse. The polio policy developed during 1937 was maintained and modified over the next decade, and expanded into the most comprehensive in the country.
By the end of the second wave of major polio epidemics in Canada a high degree of provincial government interest had developed in the treatment, hospitalization and unconditional financial support of those stricken by this tragic disease. The unprecedented polio crisis of 1937 in Ontario, its middle class impact, and the very limited prospects for prevention, had generated an expanded program in state medicine. The previous experience of other provinces with epidemic polio, particularly Alberta in 1927-28 and Manitoba in 1936, had established important precedents in the unconditional deployment of free diagnostic and treatment programs by provincial governments. In most provinces, as polio epidemics worsened into the 1940s, and especially into the 1950s, such government treatment programs evolved into specific and often sophisticated provincial polio policies. Their expansion was also driven by the prominent example of the unconditional patient treatment program of the National Foundation for Infantile Paralysis in the United States. The interest of Ottawa in the polio problem also grew, especially after World War II, catalyzed by the general post-war expansion of the federal government, and by the particular personal experience and political agenda Paul Martin, who was stricken by polio in 1907 as a child, and whose son, Paul Martin Jr., became a polio victim in 1946, just prior to the elder Martin’s appointment as Minister of National Health and Welfare.(153)
This article has also stressed the importance of the close professional and personal cooperation that existed between provincial health authorities in Canada, especially in Ontario, and the public health and scientific leadership of the School of Hygiene and Connaught Laboratories in the University of Toronto. This relationship was distinctive in North America and proved highly significant to the 1937 Toronto nasal spray trial, which had important implications for the subsequent scientific understanding of polio and its human etiology. Also crucial to this relationship, particularly with respect to the treatment of polio, was the Toronto Hospital for Sick Children, and its pioneering use of standardized splints and frames, and for its "Herculean efforts" to manufacture "homemade" iron lungs in its basement. These Canadian public health, scientific and political relationships grew in importance during the next two decades and became of fundamental importance to the development, production and distribution of the Salk vaccine and the ultimate control of epidemic polio in Canada.(154) These unique factors surrounding the growing problem of polio and its control during the first half of the twentieth century thus played an influential role in justifiying and shaping the subsequent development of Canada’s public healthcare insurance system.
April 18, 2000